Types of Ileal Interposition
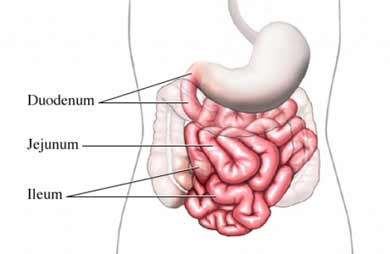
Our small intestines vary between 450 cm and 800 cm and consist of three parts: Duodenum, Jejunum and Ileum.
Duodenum creates first part of small intestines. Its length is between 20 to 25 cm. It starts just after the Pylorus muscle which controls gastric outlet. Jejunum creates second section of small intestine. Approximately 40% of small intestines is jejunum.
Ileum is the last part of small intestines. It connects small intestine into large intestine (colon). Approximately 60% of all small intestines consists of ileum.
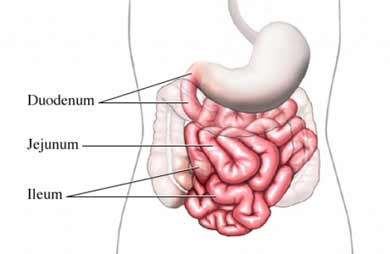 Generally, length of duodenum (around 25 cm) is not considered in average intestinal length. Therefore, length of jejunum varies between 200 to 350 cm and length of ileum varies between 350 to 450 cm. It is not possible to differentiate jejunum and ileum visually. Exact differentiation point can not be noticed. Even cellular differentiation is not on a certain point. So we base on our preliminary acceptations while determining distances.
Generally, length of duodenum (around 25 cm) is not considered in average intestinal length. Therefore, length of jejunum varies between 200 to 350 cm and length of ileum varies between 350 to 450 cm. It is not possible to differentiate jejunum and ileum visually. Exact differentiation point can not be noticed. Even cellular differentiation is not on a certain point. So we base on our preliminary acceptations while determining distances.
Small intestines are the main body part for food absorption but their functions extend beyond this. The small intestines and the digestive system has a strong hormonal impact on regulation of food absorption and process troughout the body. Different intestinal derived hormones (which are called incretins or secretins) play an important role in metabolic regulation. Therefore they have strong impact on formation and treatment of Type 2 Diabetes.
The purpose of Ileal Interposition surgeries as a sum, is to enhance the early stimulation of distal ileal segment with raw and undigested food. All tree different types of Interposition, bring the distal ileal segment to a close anatomical position in different ways.
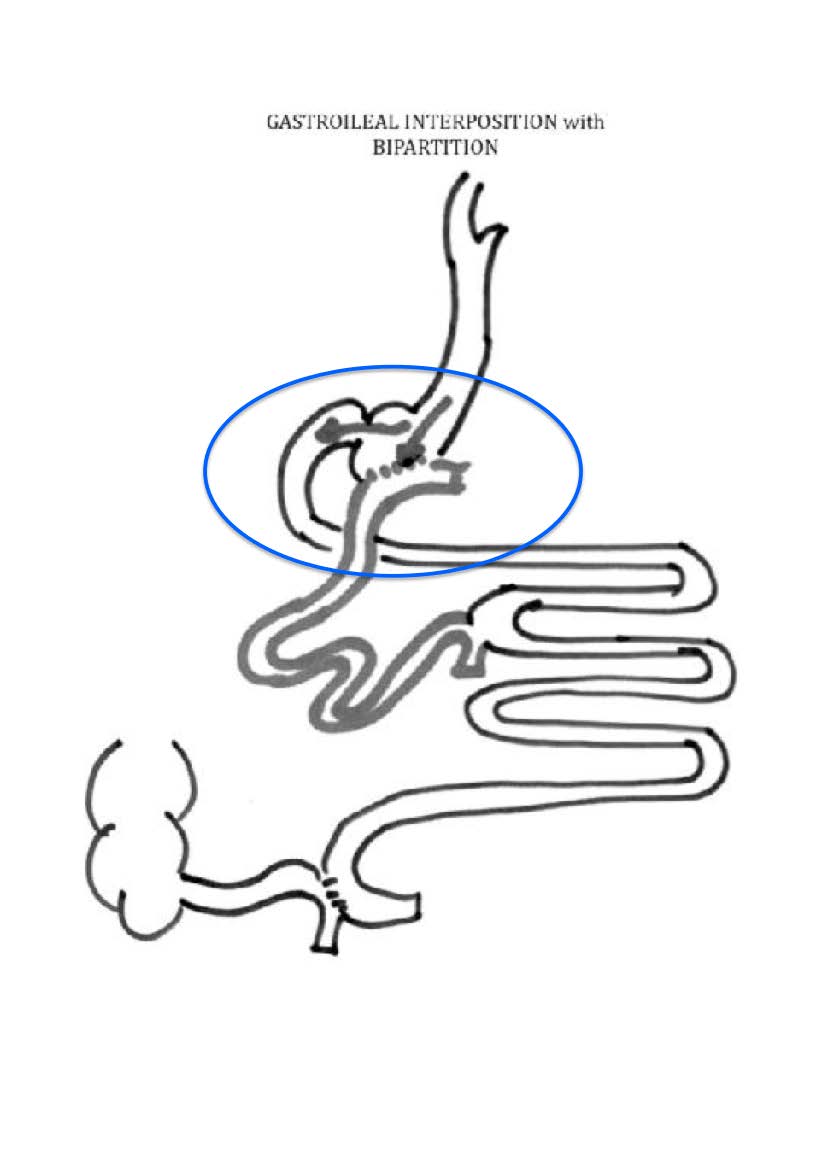
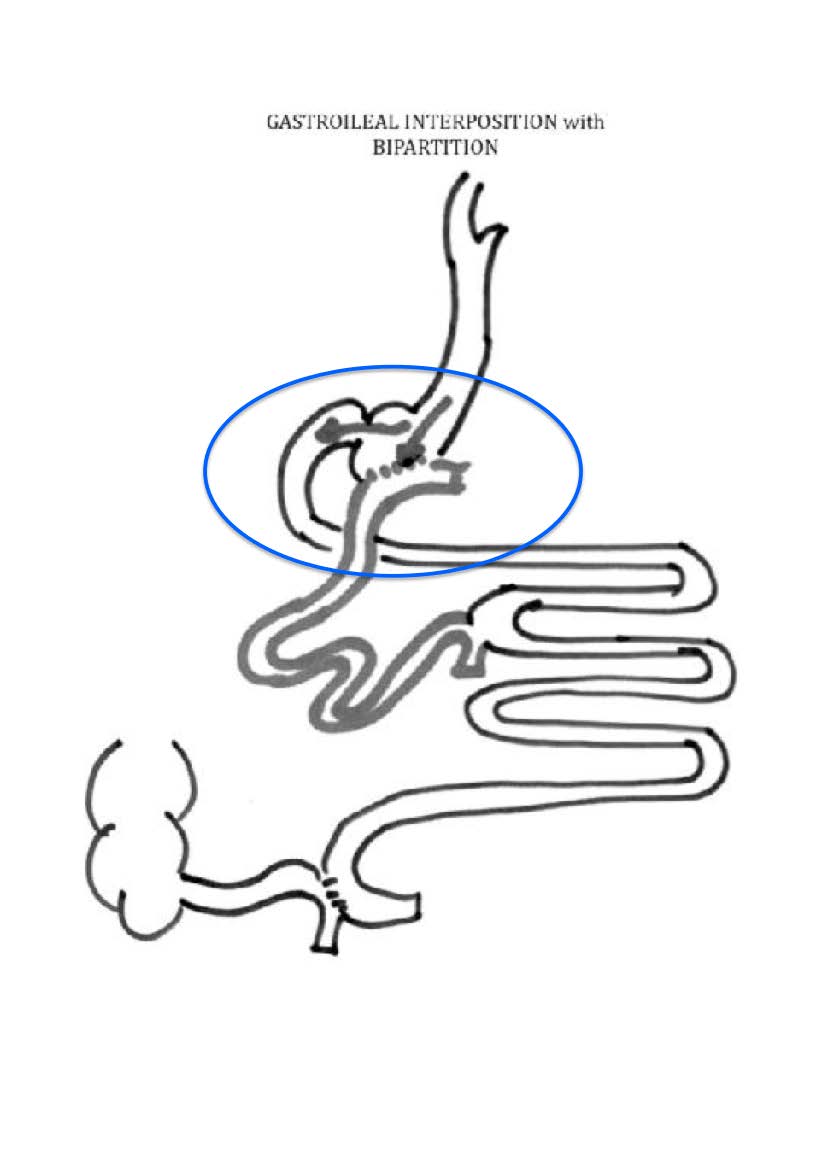
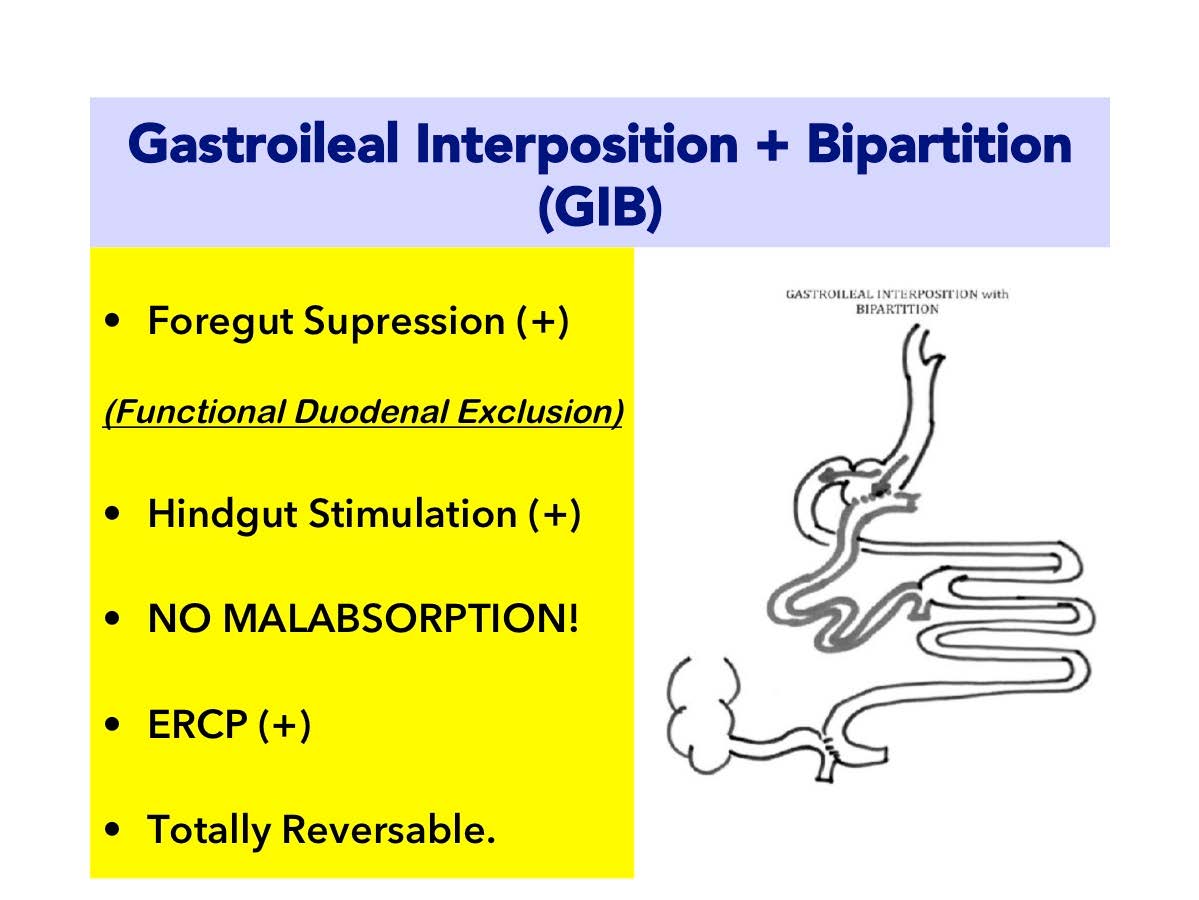
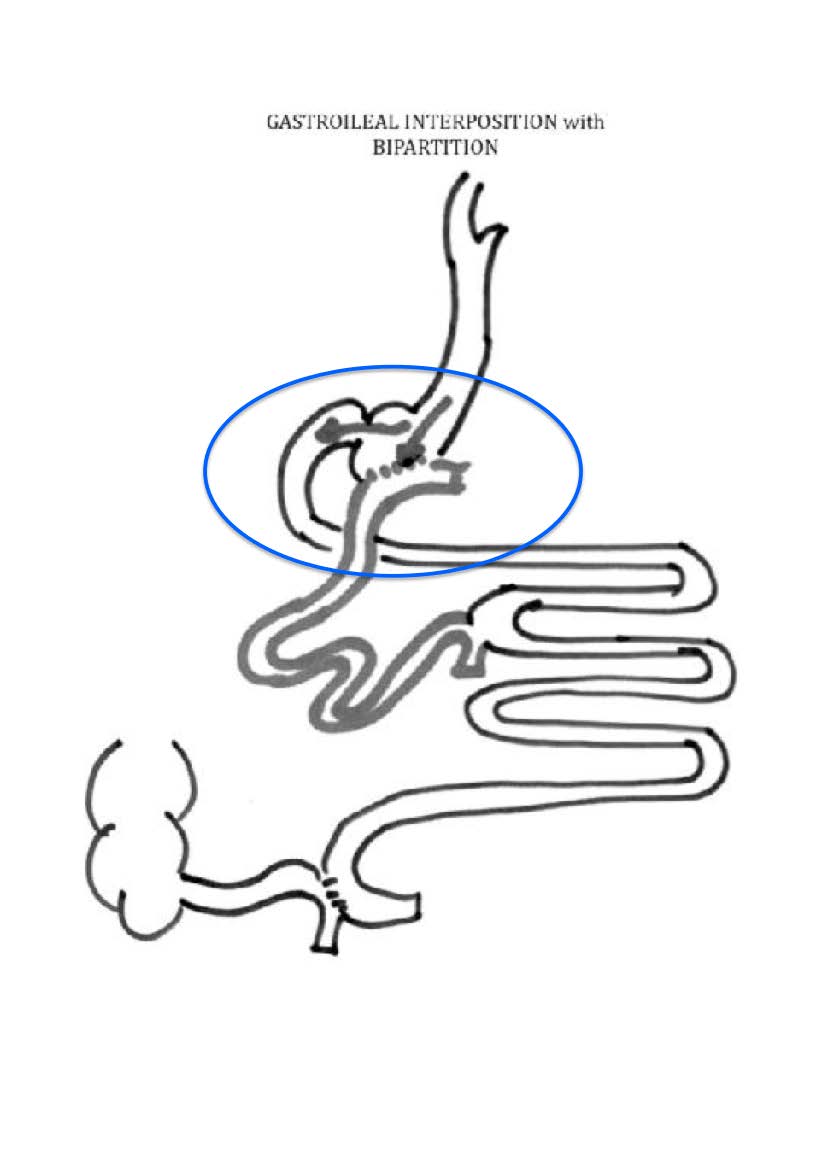
I. Gastroileal Interposition with Bipartition (GIB)
II. Duodenoileal Interposition (DII)
III. Jejunoileal Interposition (JII)
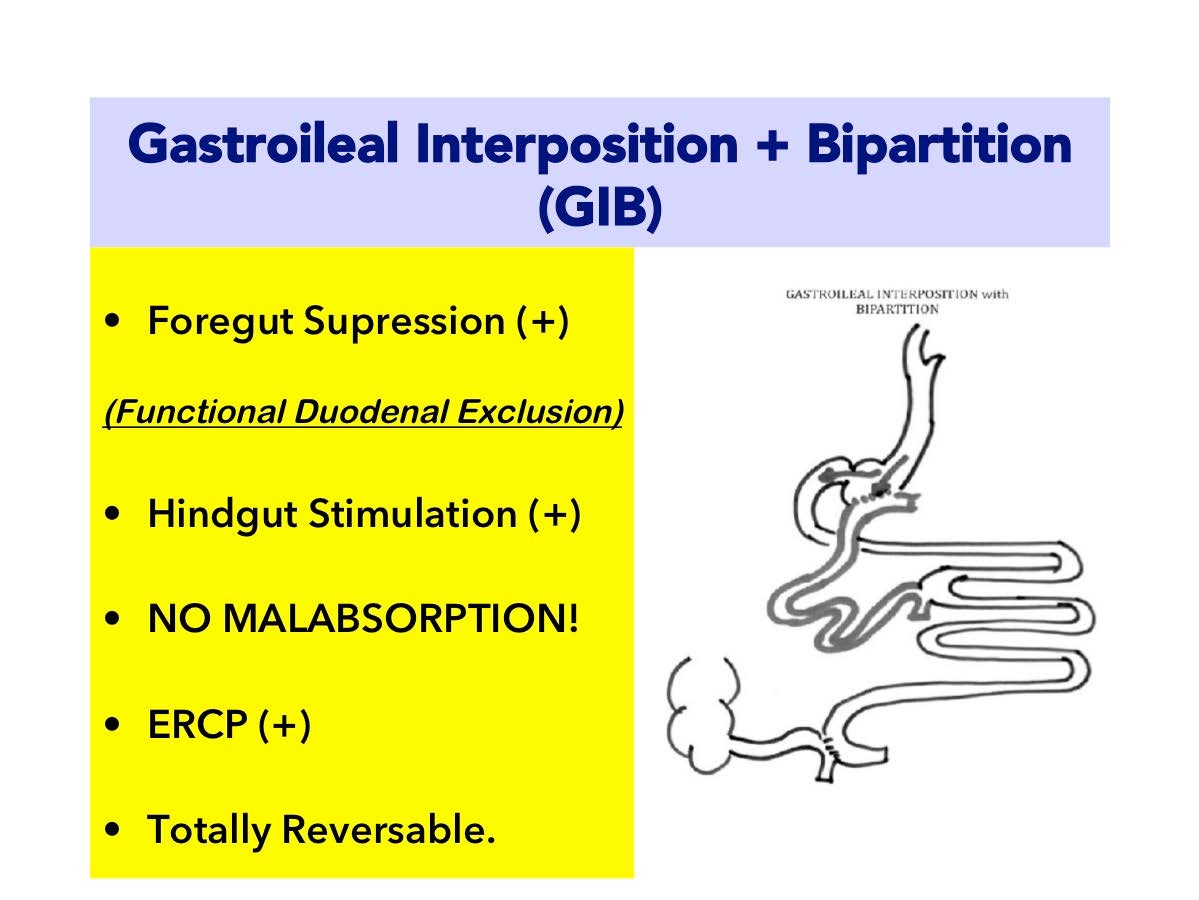
I. Gastroileal Interposition (GIB) :
a. Ileal segment is connected directly to the stomach. Early and strong stimulation of distal ileum. (HINDGUT STIMULATION)
b. Duodenal anatomy is preserved.
c. ERCP is available after surgery.
d. Large gastroileal anastomoses enhances food to be directed mainly to ileal segment. By this way duodenum is kept away from food. The negative incretin secretion is suppressed. (FOREGUT SUPRESSION!)
e. All the bowels are in contact with food. Moreover the ileal segment which becomes the main route of stomach drainage, diverts all its material to the very beginning of jejunum. That’s why there is NO MALABSORPTION RISK.
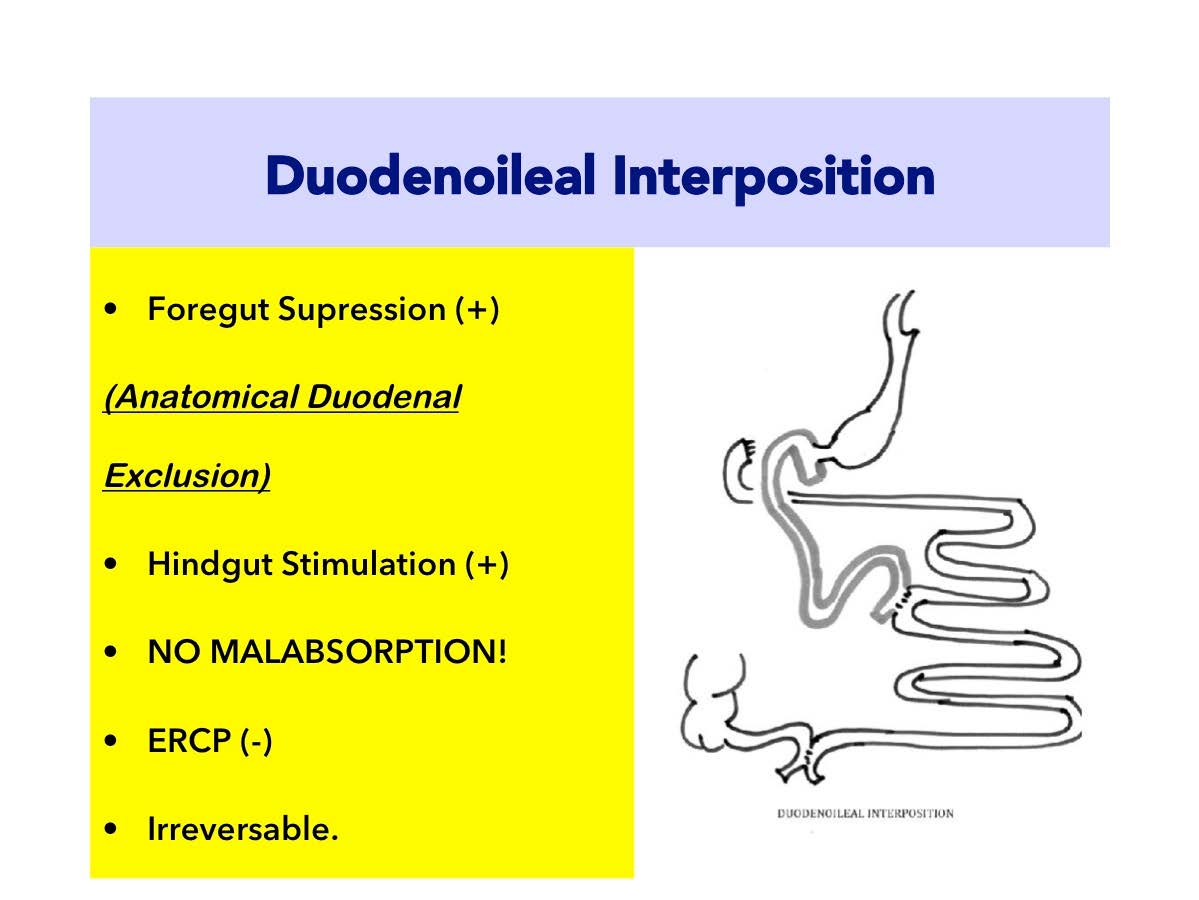
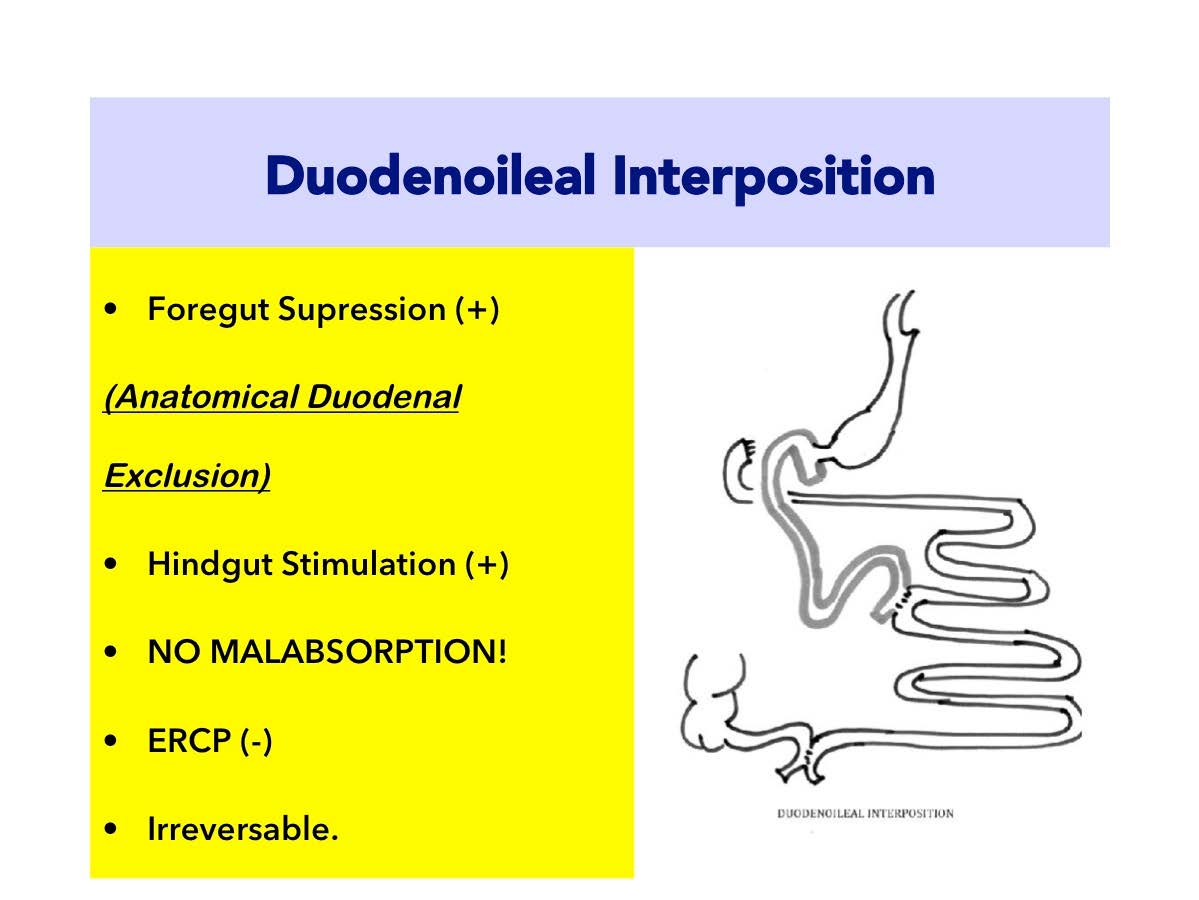
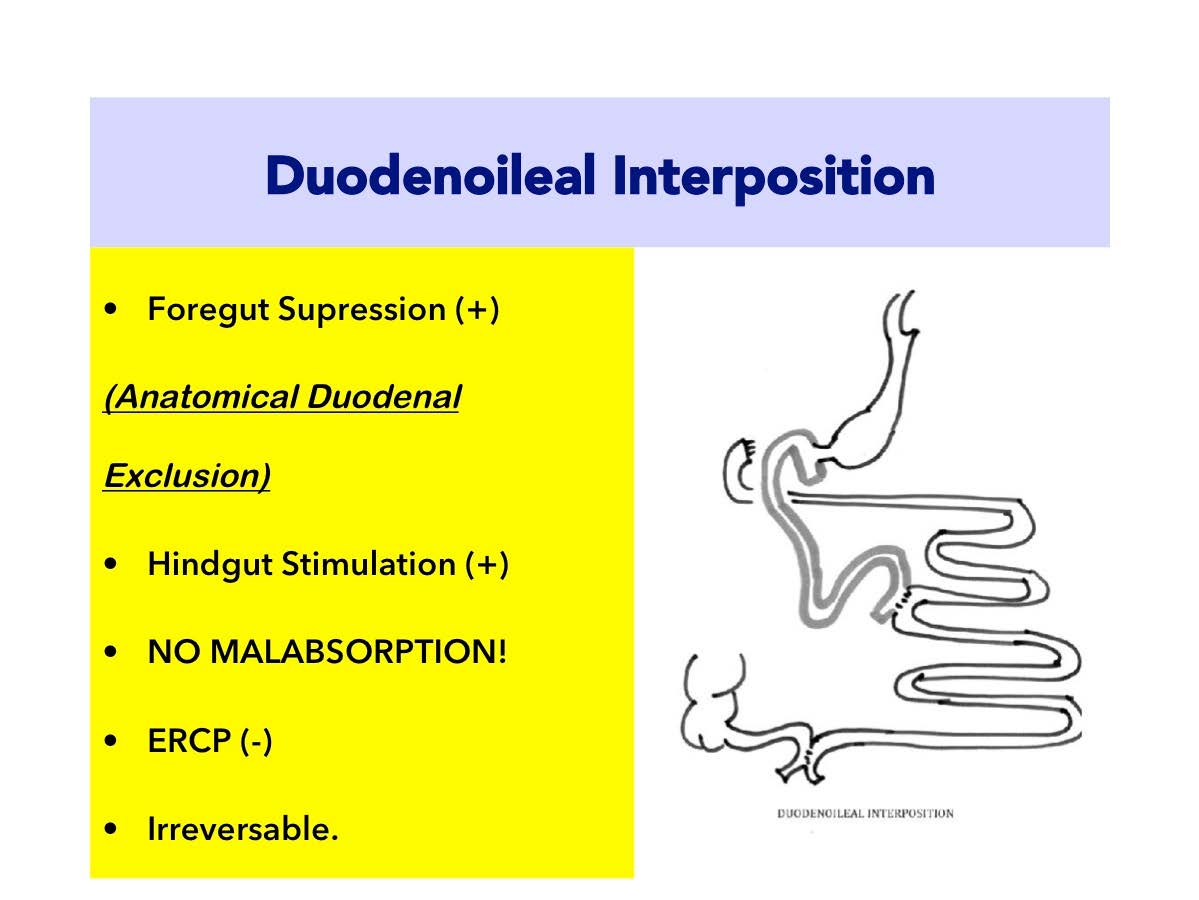
II. Duodenoileal Interposition :
a. The ileum is connected to postpyloric duodenum.
b. Duodenum is transected and diverted from food.
c. Duodenum is definetly excluded from food.
d. Strong FOREGUT SUPRESSION!
e. Strong HINDGUT STIMULATION!
f. ERCP becomes impossible due to anatomical exclusion of duodenum!
g. Its almost Irreversable.
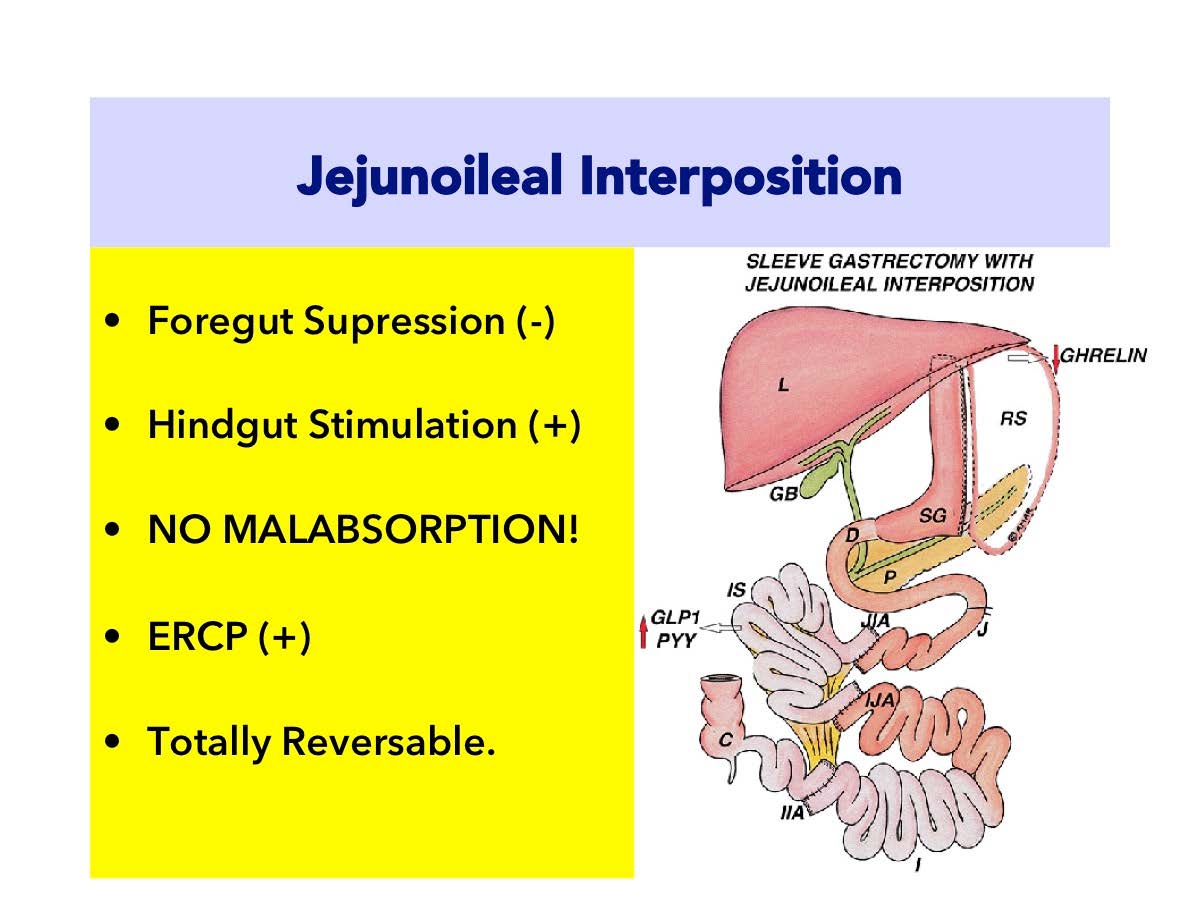
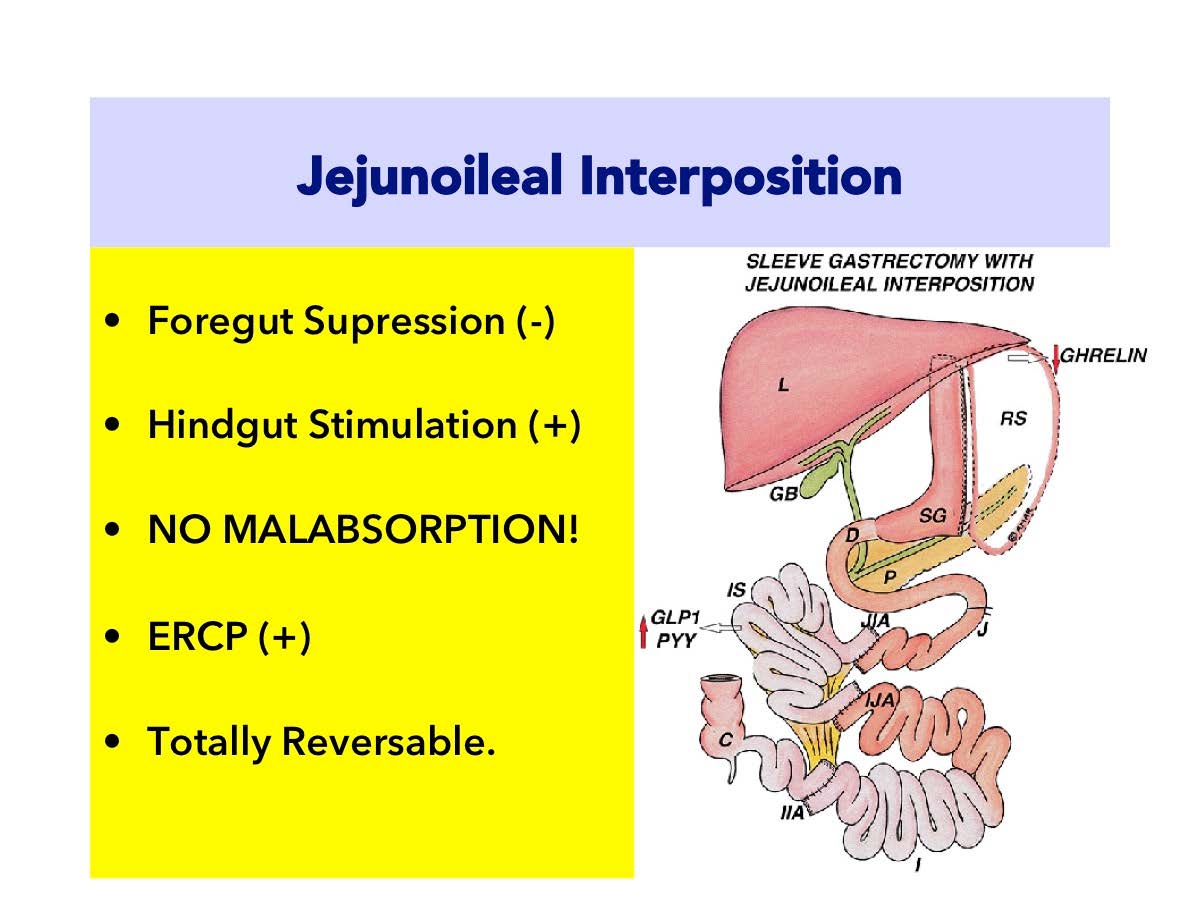
III. Jejunoileal Interposition :
a. The ileum is connected to jejunum after Treitz ligment.
b. Duodenum is preserved and stay directly connected with food.
c. NO FOREGUT SUPRESSION! (Less Antidiabetic Effect).
d. HINDGUT STIMULATION (Better than RYGB)
e. ERCP is available!
f. Totally Reversable.
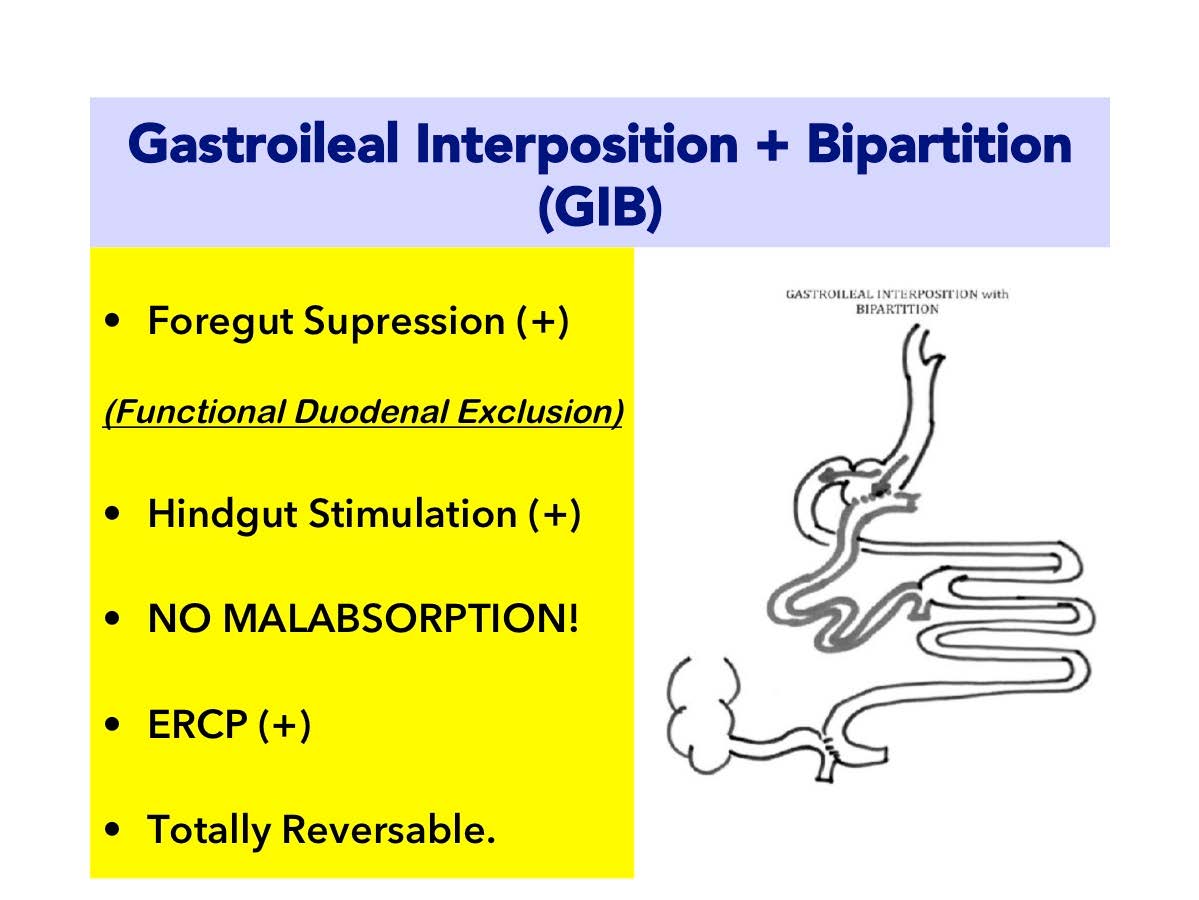
Gastroileal Interposition with Bipartition (GIB)
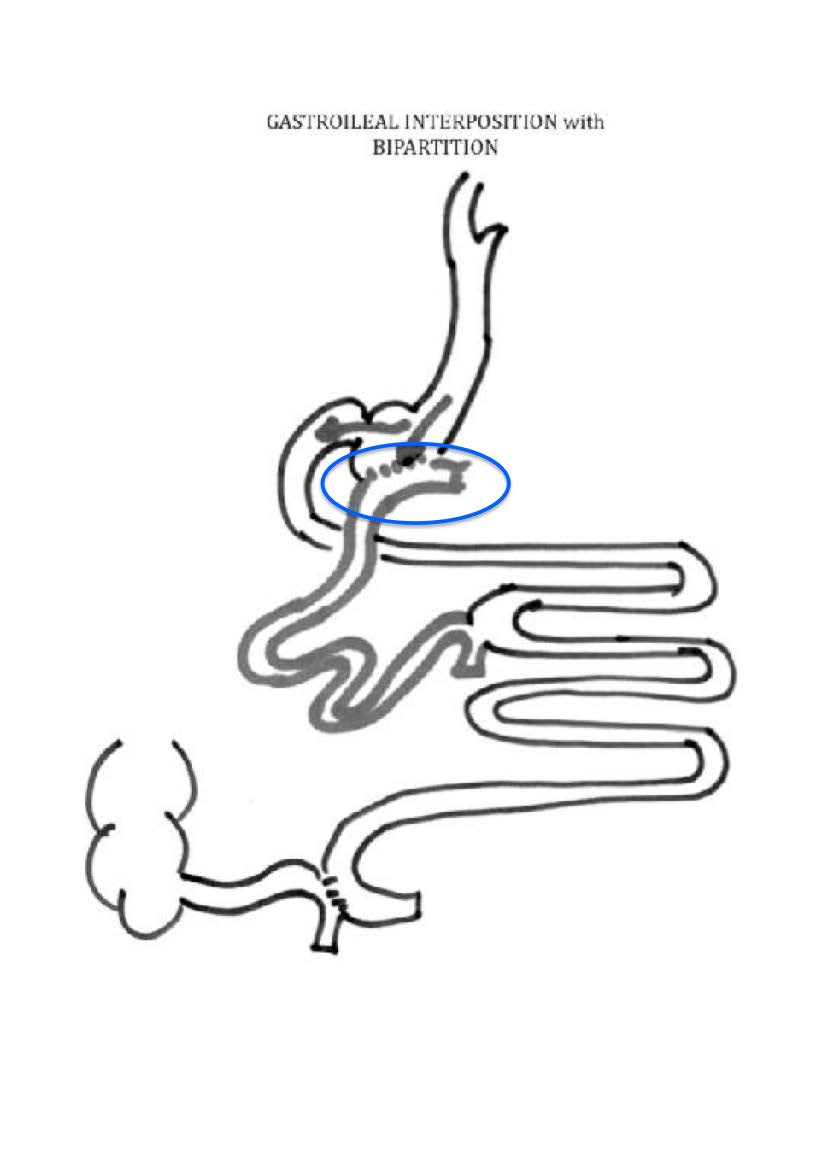
Gastroileal Interposition (GIB) is a new model of metabolic surgery that had been described by Tugrul Demirel M.D. as a salvage procedure for malnutrition after Transit Bipartition. Its based on mainly the hindgut stimulation and a functional duodenal exclusion which provokes the suppression of foregut derived negative anti-incretin secretion.
Gastroileal Interposition (GIB) :
a. Ileal segment is connected directly to the stomach. Early and strong stimulation of distal ileum. (HINDGUT STIMULATION)
b. Duodenal anatomy is preserved.
c. ERCP is available after surgery.
d. Large gastroileal anastomoses enhances food to be directed mainly to ileal segment. By this way duodenum is kept away from food. The negative incretin secretion is suppressed. (FOREGUT SUPRESSION!)
e. All the bowels are in contact with food. Moreover the ileal segment which becomes the main route of stomach drainage, diverts all its material to the very beginning of jejunum. That’s why there is NO MALABSORPTION RISK.
Advantages of GastroIleal Interposition (GIB)
Gastroileal Interposition (GIB) operation is stronger than Jejunoileal Interposition (JII) in terms of foregut suppression and hindgut stimulation. Small intestine distance is not shortened as in all Interposition surgeries. In other words, no malabsorption occurs.
The advantages are:
 1) To provide food transfer to ileum earlier than digestion. Early passage of foods to ileum, which are not mixed with bile, stimulates satiety hormones. The secretion of GLP-1 is stimulated strongly with early passage of foods to distal ileum segment. GLP-1 is rapidly released to the blood circulation. This fast GLP-1 production facilitates control of blood glucose.
1) To provide food transfer to ileum earlier than digestion. Early passage of foods to ileum, which are not mixed with bile, stimulates satiety hormones. The secretion of GLP-1 is stimulated strongly with early passage of foods to distal ileum segment. GLP-1 is rapidly released to the blood circulation. This fast GLP-1 production facilitates control of blood glucose.
GLP-1 has two important effects:
• Increases insulin production from pancreas.
• Reduces muscle and tissue resistance against insulin.
 2) To provide hormonal balance. The effect provided by GastroIleal Interposition is actually regulation of hormonal signals between small intestines and brain. By this effect, hormones creating resistance against insulin are refrained. Obstacles before insulin are removed. Your blood glucose is reduced to normal levels easily with less insulin. This phenomenon is named as “hormonal breaking” or “neuroendocrine break”.
2) To provide hormonal balance. The effect provided by GastroIleal Interposition is actually regulation of hormonal signals between small intestines and brain. By this effect, hormones creating resistance against insulin are refrained. Obstacles before insulin are removed. Your blood glucose is reduced to normal levels easily with less insulin. This phenomenon is named as “hormonal breaking” or “neuroendocrine break”.
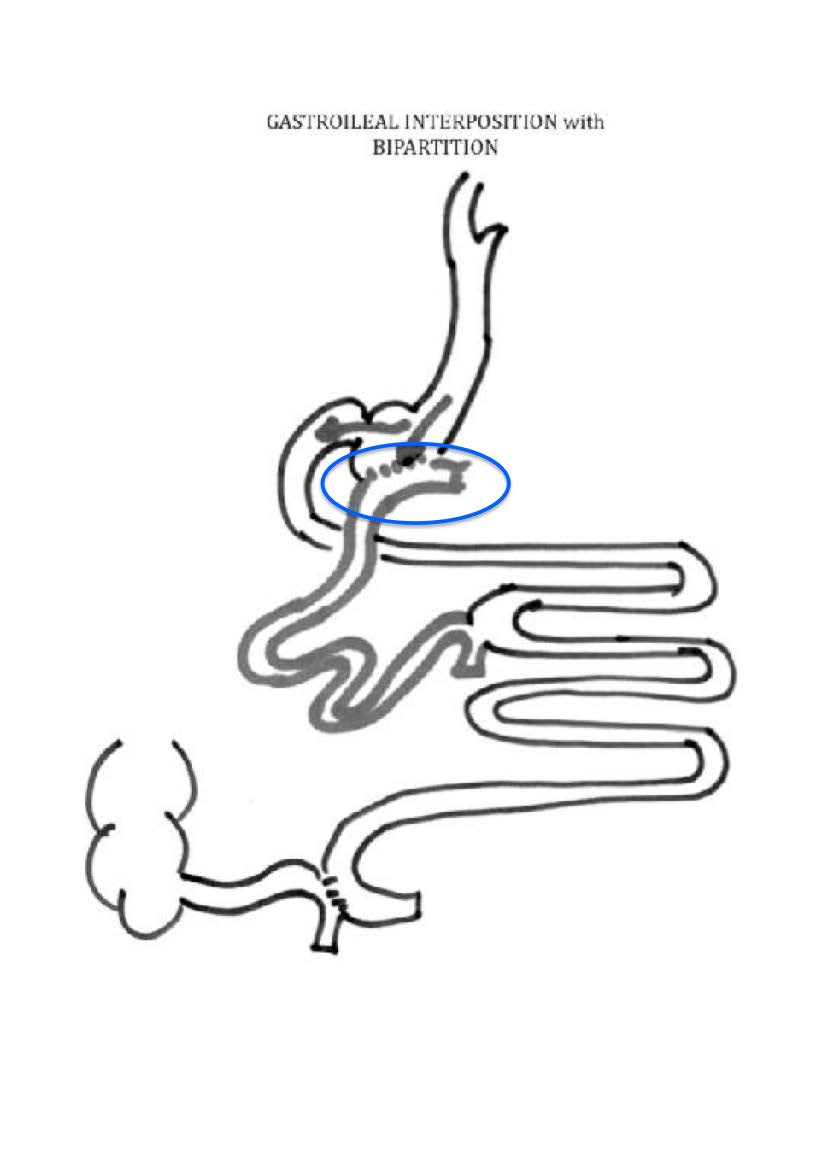 3. ERCP availability. The GIB Surgery, preserves the duodenogastric continuity while, functionally excluding duodenum from food transit. This anatomical difference from Duodenoileal Interposition, gives the patient the opportuinity to be able to preserve the availability of endoscopic evaluation for biliary problems with endoscopic retrograde colangio-pancreatography (ERCP). However, in Duodenal Switch and Duodenoileal Interposition, ERCP becomes impossible.
3. ERCP availability. The GIB Surgery, preserves the duodenogastric continuity while, functionally excluding duodenum from food transit. This anatomical difference from Duodenoileal Interposition, gives the patient the opportuinity to be able to preserve the availability of endoscopic evaluation for biliary problems with endoscopic retrograde colangio-pancreatography (ERCP). However, in Duodenal Switch and Duodenoileal Interposition, ERCP becomes impossible.
 In first step of GastroIleal Interposition (GIB), half of the stomach is removed longitudinally. The stomach is formed in a tube shape just like a sleeve gastrectomy. Sleeve Gastrectomy is an efficient obesity operation even solely. The sleeve gastrectomy performed with GastroIleal Interposition (GIB) has a hormonal target to increase the metabolic response.
In first step of GastroIleal Interposition (GIB), half of the stomach is removed longitudinally. The stomach is formed in a tube shape just like a sleeve gastrectomy. Sleeve Gastrectomy is an efficient obesity operation even solely. The sleeve gastrectomy performed with GastroIleal Interposition (GIB) has a hormonal target to increase the metabolic response.
Ghrelin hormone secreted from the fundus part which is removed triggers sense of hunger. Therefore, Ghrelin hormone is also called as “hunger hormone”. When fundus part of the stomach is removed with sleeve gastrectomy, cells which produce hunger hormone are also removed. Hunger hormone levels reduces.
Ghrelin is also a part of anti-insuliner system (working against insulin). Ghrelin plays a role in insulin resistance. Sleeve gastrectomy applied with GastroIleal Interposition (GIB) contributes to a decrease on insulin resistance.
Finally, gastric volume is partially reduced. Fullness is obtained with small portions after the operation. So calorie restriction is performed.
• Ghrelin amount known as hunger hormone decreases. Sense of fullness lasts longer.
• Insulin resistance decreases by decrease of ghrelin.
• Stomach is reduced and calorie restriction is obtained.
• Earlier passage of foods from ileum increases GLP-1 secretion.
• GLP-1 stimulates pancreas and increases insulin production.
• GLP-1 also removed insulin resistance on the tissues.
• By elimination of insulin resistance, findings of diabetes regress.
Accompanying diseases due to diabetes also recover.
Duodenoileal Interposition :
-
- Duodenum is transected and 100 % excluded from food.
- Strong FOREGUT SUPRESSION!
- The ileum is connected to post-pyloric duodenum.
- Strong HINDGUT STIMULATION!
- ERCP becomes impossible due to anatomical exclusion of duodenum!
- Its almost Irreversable.
- The Most Potent Anti-Diabetic Effect!
Duodenoileal Interposition (DII)
Duodenoileal Interposition (DII) is the first metabolic surgery that was specifically designed to treat Type 2 Diabetes (T2DM) patients with BMI<35 kg/m2 by Dr.Aureo Ludovico De Paula from Brazil in 2006. It is almost a “non-malabsorptive” procedure diverting the food to the 40-50 cm of Treitz, to proximal jejunum. This is just the same as standart Roux-en-Y Gastric Bypass (RYGB). But in RYGB food is transfered to the jejunum directly and ileum is still all the way down the whole intestinal length. In this way, RYGB is 100 % a “Foregut” surgery, but stimulation of hindgut is weak. Where as Duodenoileal Interposition (DII) brings the very distal ileal segment to the exit of stomach to have a potent hindgut stimulation. As the duodenum is transected and anatomically excluded, Duodenoileal Interposition (DII) has also a potent effect on “foregut” suppression of negative incretins.
Duodenoileal Interposition (DII) : The Metabolic Effect
Duodenoileal Interposition (DII) is the most potent anti-diabetic surgery with strong foregut suppression and hindgut stimulation. More over, it is as non-malabsorptive as gastric bypass, excluding only duodenum and the first 40 to 50 cm of jejunum.
- Duodenoileal Interposition(DII): Mechanisms of Action
Duodenal Exclusion (FOREGUT SUPRESSION)
Duodenum is the very first part of small intestines and has strong bonds with vital neighbour structures such as pancreas, biliary tract, hepatopancreatic vessels. It is the main part that digestion starts. The food meets at first sight, the biliary-pancreatic juice in duodenum and carbs start to be absorbsed.
Besides these digestive functions, duodenum has important regulatory hormonal effects on the energy metabolism. The negative incretins, normally balance the over-extending effect of first phase insülin reaction to absorption of glucose to inhibit life-treatening hypoglycemia. But in diabetes condition, altough the body resist the insülin hormone (leading to inefficient control of blood sugar), the the negative incretin effect of duodenum stays still and supresses more the defected insülin response. This leads to progression of diabetes. This phenomenon is called The Foregut Effect.
Duodenoileal Interposition (DII) anatomically excludes duodenum from pylorus just as the Duodenal Switch procedure. By this anatomical exclusion of duodenum, the negative incretin effect is definitely suppressed. Therefore Duodenoileal Interposition (DII) is a potent FOREGUT SUPRESSION effect.
Ileal Stimulation. (HINDGUT STIMULATION)
The ileum is the last part of small intestines and is rich in L-cells which is responsible from the secretion of Gulucagonlike Polypeptide 1 (GLP-1) and also PYY. GLP-1 and PYY are called “satiety” hormones. GLP-1 has spesific effects to support insülin action on the body. It decreases insülin resistance in muscle, liver, brain and kidneys. GLP-1 also decreases beta cell apopitosis (cell deaths) in pancreas and provokes the new beta cell formation.
The most potent HINDGUT Stimulating procedures are the Biliopancreatic Diversion(BPD) and Duodenal Switch (DS) operations. Duodenoileal Interposition (DII) is as potent as BPD and DS on hindgut stimulation. The undigested food is immediately transferred to very distal ileal segment after pylorus muscle. This is even before it meets the biliopancreatic juice. This early ileal stimulation, provokes strong GLP-1 production and control of the disease.
The Neuro-Endocrine Break
Duodenoileal Interposition (DII) is purely a metabolic surgery. This is because it does not lean on gastric restriction/anastomotic diameter as RYGB and not malabsorptiveas BPD/DS.
Duodenoileal Interposition (DII) can therefore be described as an endocrine surgery which has no anatomical restrictions or malabsorption. It has hormonal targets in all steps. The most potent and prominent one of them is the interposition of ileum. This provokes a sudden and strong GLP-1 stimulation which is proved to be long-lasting over 20 years in similar operations. This GLP-1 secretion effects locally and systematically:
Locally on gastrointestinal system, GLP-1 supresses the motility of the food in digestive system which enhances the feeling of satiety.
Systematically on all targets of insulin hormone such as the muscle cells, liver, brain, kidney and even intestinal mucosa to increase the insulin effects. By this way, especially in brain, the satiety is also provoked. As a sum, after the food is transferred to ileum, the “neuroendocrine effect” immediately takes place and satiety stage is reached. This phenomenon is also called as “The Hormonal Break” or “Neuroendocrine Break”.
The Hormonal Efects: Step by Step
Duodenoileal Interposition (DII) has a hormonal target in all steps of the procedure. Let’s take a look at these.
- Sleeve Gastrectomy (Removal of Fundus – Gherelin Control)
A weight adjusted sleeve gastrectomy is included as a first step in Duodenoileal Interposition (DII). The sleeve gastrectomy does not aim to restrict the amount of food that can be consumed, but aims to do two main modification:
- To enhance the drainage of stomach to over-come the strong inhibition of gastric motility due to neuroendocrine break.
- To decrease the secretion of gherelin at the beginning. As the ghrelin is a part of the anti-insulinar system, the inhibition of secretion helps to decrease the glucose toxicity of the patient.
- Duodenal Exclusion
As the duodenum provokes also anti-insulin hormonal secretions, excluion of duodenum naturally stimulates the insülin actions on all over the body. By the duodenal exclusion, the negative incretins are supressed and insülin resistance is decreased.
- Ileal Interposition
The ileal interposition is the main part of the operation. By the help of this anatomical change, the food ingredient of stomach, can be easily delivered to the very distal part of the small intestines where they can strongly stimulate the L-cells to produce GLP-1 and PYY, the so called satiety hormones. The neuroendocrine break evokes in this way to have local and systematic actions to fix the insülin resistance.
Is Duodenoileal Interposition (DII) malabsorptive?
Totally Non-Malabsorptive Surgery
This is the most important point that we should discuss about Duodenoileal Interposition (DII). Let’s go over again the RYGB (Roux-n-Y Gastric Bypass) which is almost a non-malabsorptive surgery. In RYGB, whole stomach, whole duodenum and up to 50 cm of jejunum are bypassed. The whole intestinal length of a humanbeing might be in between 350 cm to 1100 cm long. So even in the shortest length of bowels (around 350 cm), RYGB can only bypass 1/7th of the intestines (14.2 % approx.). This means that the 85% of the intestines are in direct contact with food and absorption process. In patients who have longer intestinal lengths, such as 800 cm, the malabsorptive “bypassed” intestinal length gets much more shorter to 1/16th (6.25 %approx.) of all the bowels.That’s why malabsorption becomes neglectable. RYGB patients only needs iron and to some extend B12 replacements as their tiny pouches preserve its volume (40-50 cc approx.). As the pouch enlarges, the patients start to feel more hunger, and feel the increase in portions. Those patients mostly do not need any replacement cause the ingested food becomes available to maintain iron and B12 levels. But this is also related with significant loss of the effect of the RYGB procedure, with weight regain and recurrence of diabetes.
Duodenoileal Interposition (DII) has a similar anatomical bypass comparable with RYGB. Duodenoileal Interposition (DII) also bypasses whole stomach, whole duodenum and up to 50 cm of jejunum. So the malabsorptive compartment is limited to 6-10 % of all bowel length. This is expected to provoke some iron and B12 deficiency but in more than 85 % of DII patients, even these are not present. The main difference is the capacity of stomach to consume. When compared to RYGB pouch of 40-50 cc, the remaining stomach volume of DII is more than 200 cc at the very early post operative period. As the time pass, the stomach volume increases to a capacity more allowing up to almost a meal portion. The impact of the DII does not lean on the stomach restriction and anastomotic diameter as in RYGB. However DII has a strong “neuroendocrine hormonal break” system that provokes hormonal satiety and gastrointestinal motility control which limits the amount of food consumed and triggers insulin sensitivity in all body cells.
Duodenoileal Interposition (DII) has no anatomical limitations on restriction of volume or anastomotic diameter. DII is beyond all of these limitations, acting solely on hormonal issues which enhances by the time as the L-cells increase with early contact with undigested food.
Jejuno-Ileal Interposition (JII)
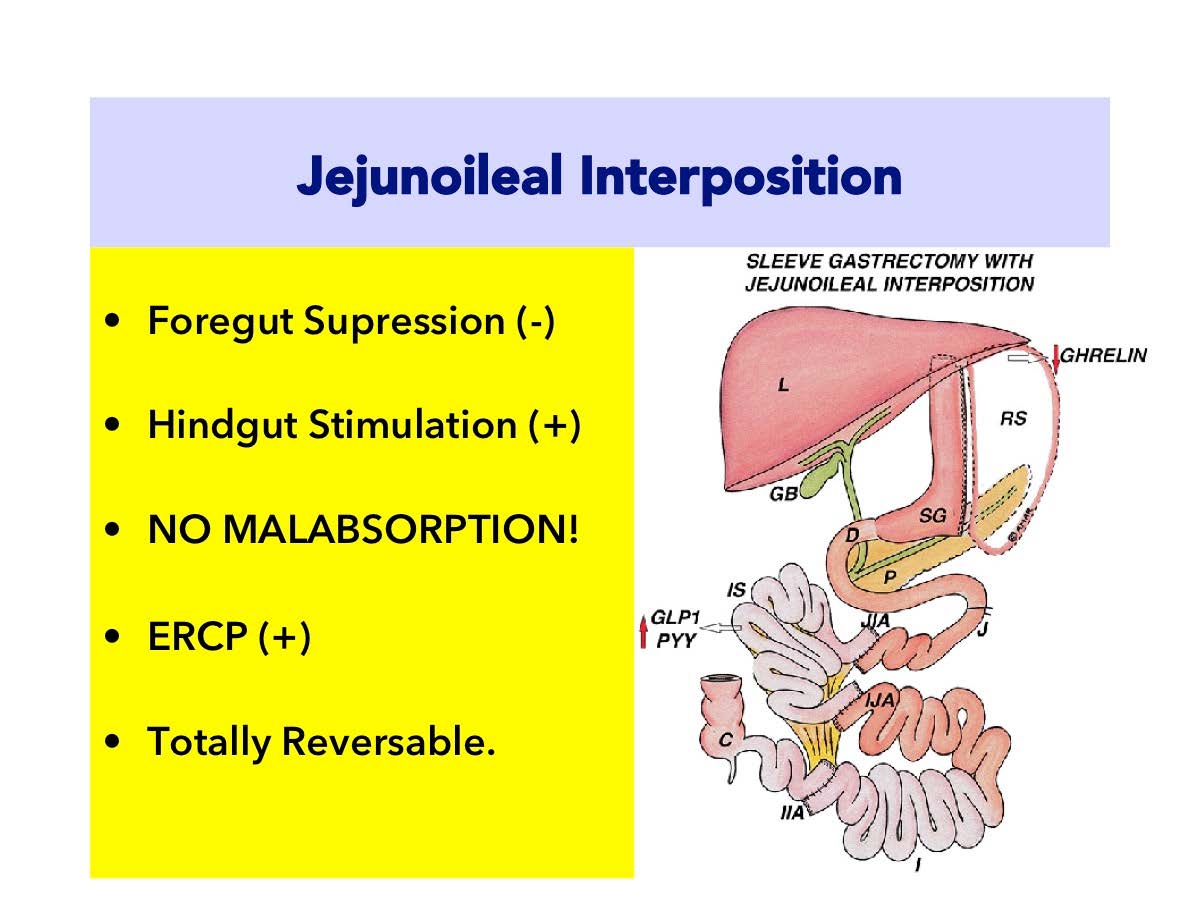
The purpose of Jejuno-Ileal Interposition (JII) is to change order of food transit in your small intestines.The aim of the JII is to make food to contact with ileum which is the last part of our small intestines in an earlier stage after consumption.
Jejuno-Ileal Interposition (JII) is the replacement of terminal part of the small intestines (ileum) with medial part (jejunum).
Outer part of the stomach is removed vertically as in sleeve gastrectomy and the pylorus muscle which is specialized to control gastric exit is preserved.Gastric connection of duodenum is not interrupted. Normal anatomy is preserved.
As seen in the figure, a 170 cm part from ileum which is the distal (last) part of the small intestines, is transected.Ends of remaining two parts of small intestine are connected to each other and continuity is provided. Jejunum is separated at 30-40 cm at the beginning of Treitz ligament.Upper end of ileum which is separated and liberated is connected to upper end of jejunum; lower end of ileum is connected to lower end of jejunum.So, foods passing from the stomach comes to ileum after a short distance from duodenum (25 cm).
Duodenum (the small intestine part just after the stomach) is kept as it is.Bile flow is not interrupted.However, ileum part which is about 300-400 cm far from stomach is brought to 50 cm away.So, foods consumed come to ileum after a short period and without being digested completely and start L-cell stimulation.
Jejuno-Ileal Interposition (JII): Metabolic Power of Action
Jejuno-Ileal Interposition (JII) operation is purely a metabolic surgery which acts on hormonal bases. However, weaker than Duodeno-Ileal Interposition (DII) especially by means of duodenal transection, it is still as effective as RYGB (Roux-n-Y Gastric Bypass). The RYGB is almost purely a FOREGUT suppressing surgery, where asJejuno-Ileal Interposition (JII) is stimulating HINDGUT. Both procedures (RYGB and JII) have pros and cons to each other but, the absence of a blind stomach pouch in JII makes it more superior in patients who has gastric cancer in family history. Also, small intestine distance is not shortened in Jejuno-Ileal Interposition (JII) operation.In other words, no absorption defect occurs.
Jejuno-Ileal İnterposition (JII): Step by Step
- Sleeve Gastrectomy: The Vertical Sleeve Gastrectomy is applied as weight adjusted. This means patients with severe obesity needs more restriction, where as low BMI patients needs more eating capacity. This is adjusted differently in different patients. The major aim of the sleeve is to re-shape the stomach to enhance its drainage to intestines. otherwise with out a sleeve gastrectomy, the interposed ileal segment may provoke gastric stasis and discomfort. This is due to “neuro-endocrine break” that is provoked by GLP-1 from stimulated L-cells.
Ghrelin hormone is secreted from the fundus part of the stomach and triggers sense of hunger.Therefore, Ghrelin hormone is also called as “hunger hormone”.When fundus part of the stomach is removed with sleeve gastrectomy, cells which produce hunger hormone are also removed.Hunger hormone levels goes down.
Ghrelin is also a part of anti-insuliner system (working against insulin).Therefore Ghrelin also plays a role in insulin resistance.Sleeve gastrectomy applied with Jejuno-Ileal Interposition (JII) contributes to a significant decrease on insulin resistance.
2) Ileal Interposition. Early passage of foods which are not “completely mixed” with bile to ileum stimulates GLP-1 and PYY hormones.These hormones are secreted from ileum and stimulated strongly with early passage of foods.GLP-1 is rapidly released to the blood circulation.This fast GLP-1 production facilitates control of blood glucose.GLP-1 has two important effects:
- Increases insulin production from pancreas.
- Reduces resistance of muscles and tissues against insulin.
3)Hormonal Balance.The effect provided by Jejuno-Ileal Interposition (JII) is actually the regulation of hormonal signals between small intestines and brain. By this, anti-insulinar hormonal system is controlled. The insulin resistance is fixed.The blood glucose is reduced to normal levels easily with less insulin.This is called “hormonal break” or “Neuro-Endocrine Break”.
- Ghrelin amount known as hunger hormone decreases.Sense of fullness lasts longer.
- Insulin resistance decreases by decrease of ghrelin.
- Stomach is reduced and calorie restriction is obtained.
- Earlier passage of foods from ileum increases GLP-1 secretion.
- GLP-1 stimulates pancreas and increases insulin production.
- GLP-1 also removed insulin resistance on the tissues.
- By elimination of insulin resistance, findings of diabetes regress.
Accompanying diseases due to diabetes also recover.
The Rubik's Cube seems to be an impossible puzzle but it's easy to solve using just a few algorithms.
 Generally, length of duodenum (around 25 cm) is not considered in average intestinal length. Therefore, length of jejunum varies between 200 to 350 cm and length of ileum varies between 350 to 450 cm. It is not possible to differentiate jejunum and ileum visually. Exact differentiation point can not be noticed. Even cellular differentiation is not on a certain point. So we base on our preliminary acceptations while determining distances.
Generally, length of duodenum (around 25 cm) is not considered in average intestinal length. Therefore, length of jejunum varies between 200 to 350 cm and length of ileum varies between 350 to 450 cm. It is not possible to differentiate jejunum and ileum visually. Exact differentiation point can not be noticed. Even cellular differentiation is not on a certain point. So we base on our preliminary acceptations while determining distances.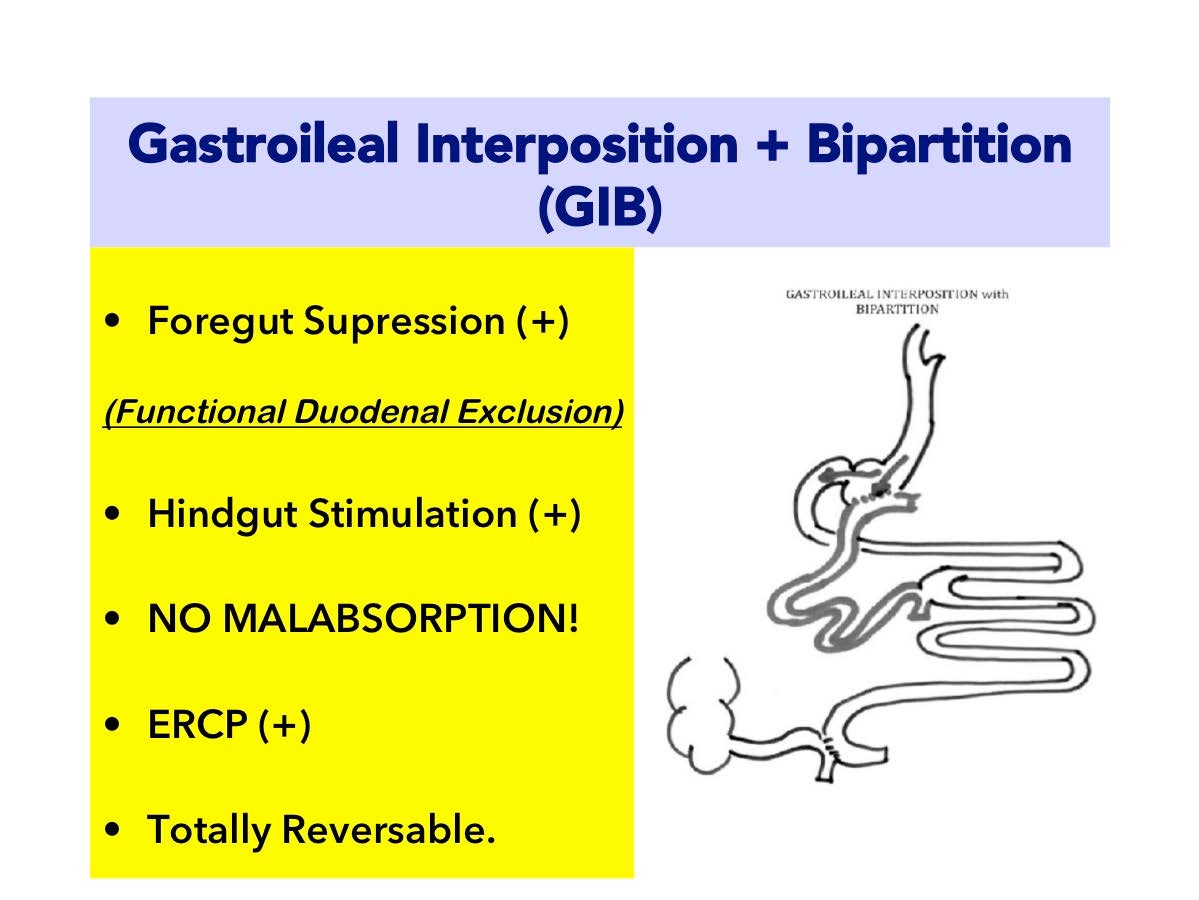
 English
English Turkish
Turkish
 1) To provide food transfer to ileum earlier than digestion. Early passage of foods to ileum, which are not mixed with bile, stimulates satiety hormones. The secretion of GLP-1 is stimulated strongly with early passage of foods to distal ileum segment. GLP-1 is rapidly released to the blood circulation. This fast GLP-1 production facilitates control of blood glucose.
1) To provide food transfer to ileum earlier than digestion. Early passage of foods to ileum, which are not mixed with bile, stimulates satiety hormones. The secretion of GLP-1 is stimulated strongly with early passage of foods to distal ileum segment. GLP-1 is rapidly released to the blood circulation. This fast GLP-1 production facilitates control of blood glucose.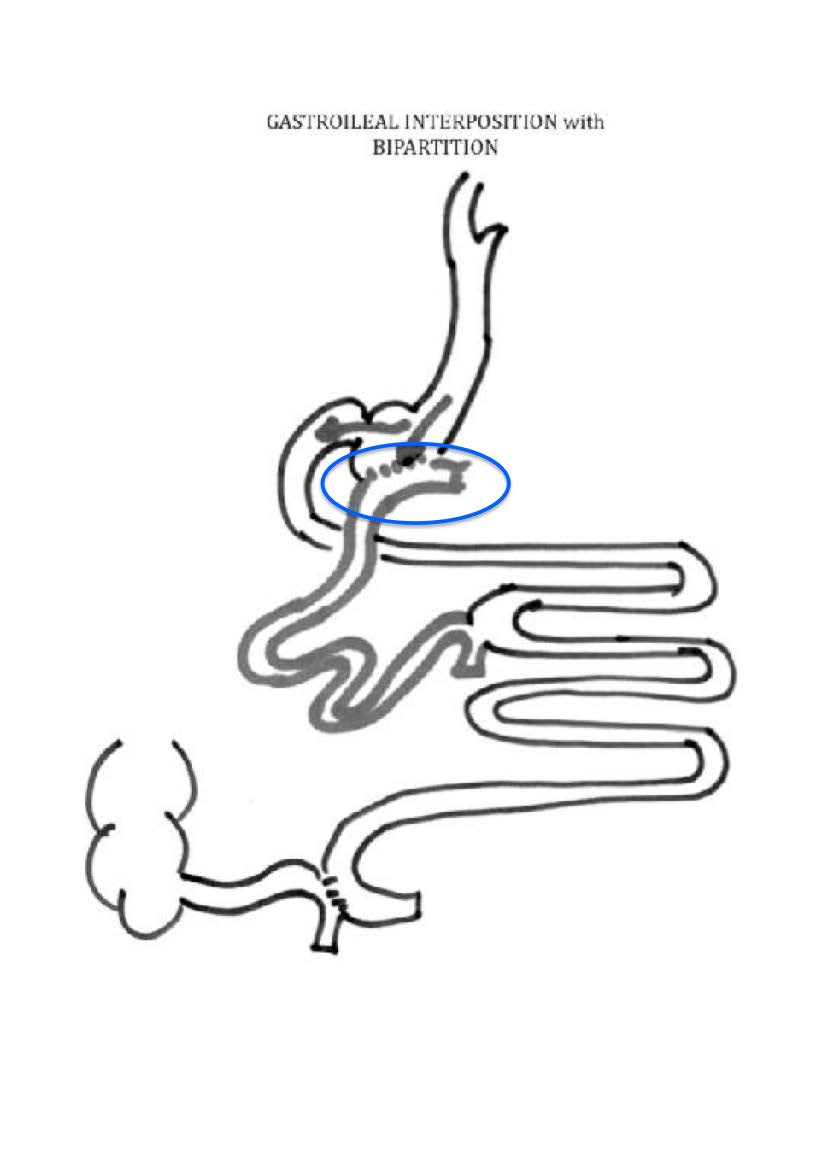 2) To provide hormonal balance. The effect provided by GastroIleal Interposition is actually regulation of hormonal signals between small intestines and brain. By this effect, hormones creating resistance against insulin are refrained. Obstacles before insulin are removed. Your blood glucose is reduced to normal levels easily with less insulin. This phenomenon is named as “hormonal breaking” or “neuroendocrine break”.
2) To provide hormonal balance. The effect provided by GastroIleal Interposition is actually regulation of hormonal signals between small intestines and brain. By this effect, hormones creating resistance against insulin are refrained. Obstacles before insulin are removed. Your blood glucose is reduced to normal levels easily with less insulin. This phenomenon is named as “hormonal breaking” or “neuroendocrine break”.
