Jejuno-Ileal Interposition (JII)
The purpose of Jejuno-Ileal Interposition (JII) is to change order of food transit in your small intestines. The aim of the JII is to make food to contact with ileum which is the last part of our small intestines in an earlier stage after consumption.
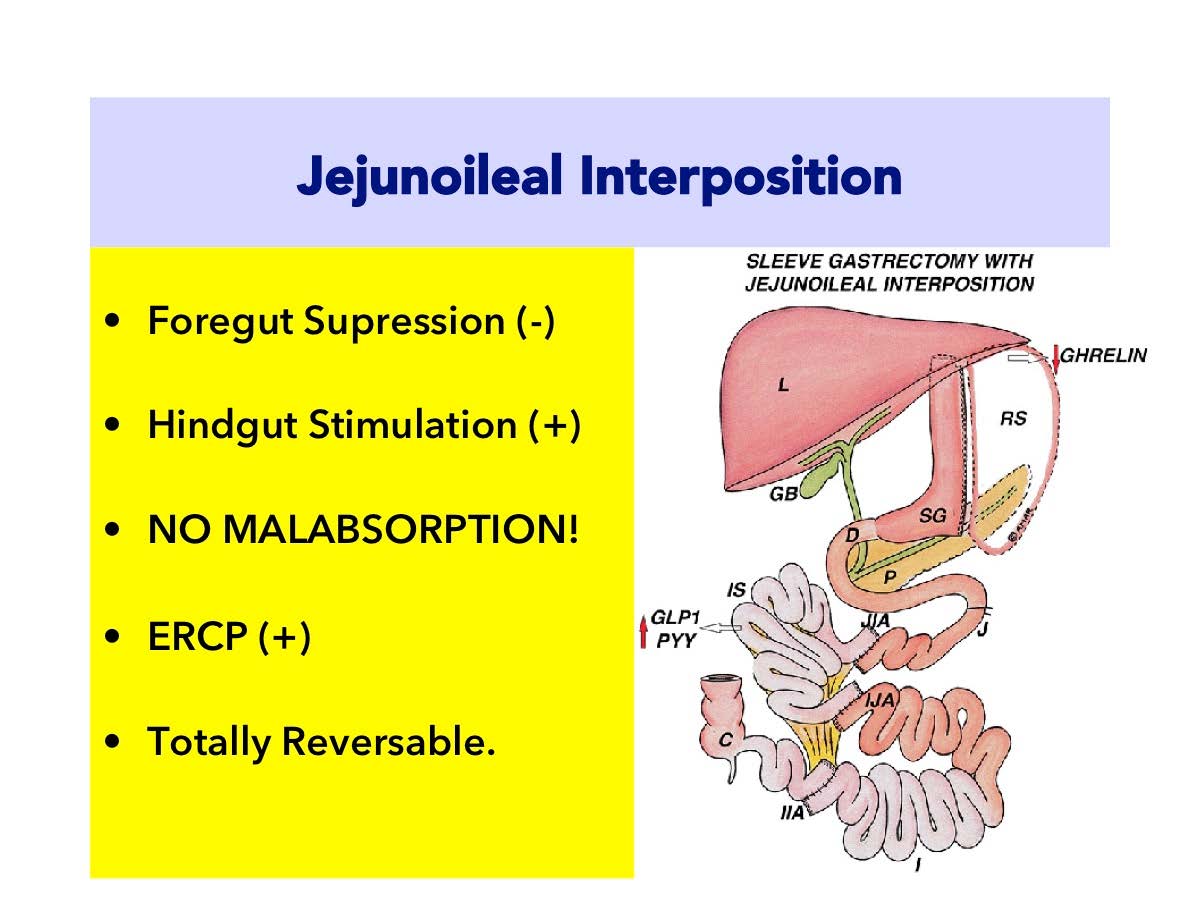
Jejuno-Ileal Interposition (JII) is the replacement of terminal part of the small intestines (ileum) with medial part (jejunum).
Outer part of the stomach is removed vertically as in sleeve gastrectomy and the pylorus muscle which is specialized to control gastric exit is preserved. Gastric connection of duodenum is not interrupted. Normal anatomy is preserved.
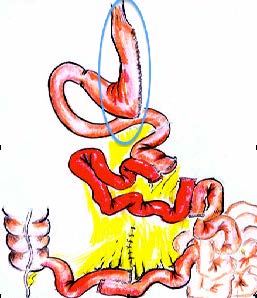
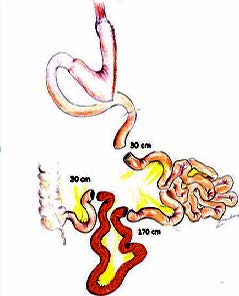 As seen in the figure, a 170 cm part from ileum which is the distal (last) part of the small intestines, is transected. Ends of remaining two parts of small intestine are connected to each other and continuity is provided. Jejunum is separated at 30-40 cm at the beginning of Treitz ligament. Upper end of ileum which is separated and liberated is connected to upper end of jejunum; lower end of ileum is connected to lower end of jejunum. So, foods passing from the stomach comes to ileum after a short distance from duodenum (25 cm).
As seen in the figure, a 170 cm part from ileum which is the distal (last) part of the small intestines, is transected. Ends of remaining two parts of small intestine are connected to each other and continuity is provided. Jejunum is separated at 30-40 cm at the beginning of Treitz ligament. Upper end of ileum which is separated and liberated is connected to upper end of jejunum; lower end of ileum is connected to lower end of jejunum. So, foods passing from the stomach comes to ileum after a short distance from duodenum (25 cm).
Duodenum (the small intestine part just after the stomach) is kept as it is. Bile flow is not interrupted. However, ileum part which is about 300-400 cm far from stomach is brought to 50 cm away. So, foods consumed come to ileum after a short period and without being digested completely and start L-cell stimulation.
Jejuno-Ileal Interposition (JII): Metabolic Power of Action 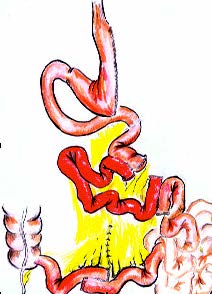
Jejuno-Ileal Interposition (JII) operation is purely a metabolic surgery which acts on hormonal bases. However, weaker than Duodeno-Ileal Interposition (DII) especially by means of duodenal transection, it is still as effective as RYGB (Roux-n-Y Gastric Bypass). The RYGB is almost purely a FOREGUT suppressing surgery, where as Jejuno-Ileal Interposition (JII) is stimulating HINDGUT. Both procedures (RYGB and JII) have pros and cons to each other but, the absence of a blind stomach pouch in JII makes it more superior in patients who has gastric cancer in family history. Also, small intestine distance is not shortened in Jejuno-Ileal Interposition (JII) operation. In other words, no absorption defect occurs.
Jejuno-Ileal İnterposition (JII): Step by Step
- Sleeve Gastrectomy: The Vertical Sleeve Gastrectomy is applied as weight adjusted. This means patients with severe obesity needs more restriction, where as low BMI patients needs more eating capacity. This is adjusted differently in different patients. The major aim of the sleeve is to re-shape the stomach to enhance its drainage to intestines. otherwise with out a sleeve gastrectomy, the interposed ileal segment may provoke gastric stasis and discomfort. This is due to “neuro-endocrine break” that is provoked by GLP-1 from stimulated L-cells.
Ghrelin hormone is secreted from the fundus part of the stomach and triggers sense of hunger. Therefore, Ghrelin hormone is also called as “hunger hormone”. When fundus part of the stomach is removed with sleeve gastrectomy, cells which produce hunger hormone are also removed. Hunger hormone levels goes down.
Ghrelin is also a part of anti-insuliner system (working against insulin). Therefore Ghrelin also plays a role in insulin resistance. Sleeve gastrectomy applied with Jejuno-Ileal Interposition (JII) contributes to a significant decrease on insulin resistance.
2) Ileal Interposition. Early passage of foods which are not “completely mixed” with bile to 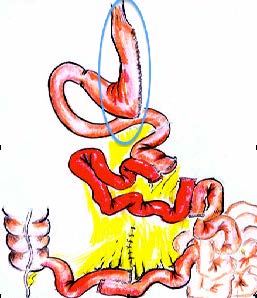 ileum stimulates GLP-1 and PYY hormones. These hormones are secreted from ileum and stimulated strongly with early passage of foods. GLP-1 is rapidly released to the blood circulation. This fast GLP-1 production facilitates control of blood glucose. GLP-1 has two important effects:
ileum stimulates GLP-1 and PYY hormones. These hormones are secreted from ileum and stimulated strongly with early passage of foods. GLP-1 is rapidly released to the blood circulation. This fast GLP-1 production facilitates control of blood glucose. GLP-1 has two important effects:
- Increases insulin production from pancreas.
- Reduces resistance of muscles and tissues against insulin.
3) Hormonal Balance. The effect provided by Jejuno-Ileal Interposition (JII) is actually the regulation of hormonal signals between small intestines and brain. By this, anti-insulinar hormonal system is controlled. The insulin resistance is fixed. The blood glucose is reduced to normal levels easily with less insulin. This is called “hormonal break” or “Neuro-Endocrine Break”.
- Ghrelin amount known as hunger hormone decreases. Sense of fullness lasts longer.
- Insulin resistance decreases by decrease of ghrelin.
- Stomach is reduced and calorie restriction is obtained.
- Earlier passage of foods from ileum increases GLP-1 secretion.
- GLP-1 stimulates pancreas and increases insulin production.
- GLP-1 also removed insulin resistance on the tissues.
- By elimination of insulin resistance, findings of diabetes regress.
Accompanying diseases due to diabetes also recover.
 English
English Turkish
Turkish