Duodenogastric Alkaline Reflux Disease (DGR)
Bile can be considered as an intestinal detergent that is vital for the body to disolve and absorb the fats in the meal. It is an important digestive fluid and produced in the liver. Liver dispenses the bile 7/24 into the duodenum with the pancreatic juice. This excretion is faster and loaded after food is ingested, especially if the gallbladder is functioning. Bile normally helps to digest lipids and inhibits the bacterial overgrowth in the small intestine. Its main component is water, and the other ingredients include bile acids, bilirubin, cholesterol, fatty acids, and lecithin. Normally, bile should meet the food in duodenum. In duodenum not only bile from liver, but also pancreatic juice and duodenal secretions also meet altogether. The stomach mucosa, although very tough to manage acid secretion, is incredibly weak against alkaline intestinal juice containing bile salts and pancreatic acids. Because of that, the pyloric sphincter has an important role preventing the bile from entering the stomach. When the pyloric sphincter is damaged or dysfunctional, bile can reflux into the stomach. That’s why its preferred to name the situation as duodenogastric reflux rather than insufficiently naming it as bile reflux. The incidence of duodenogastric reflux and its relationship with gastric and duodenal diseases are controversial.
Symptoms of Alkaline Reflux
The reflux of alkaline biliary intestinal secretion into the stomach lumen to some extend is considered as a normal physiologic phenomenon(1). However some people suffer from severe dyspeptic symptoms, pain in the stomach (epigastric pain 89%) (2), heartburn just as in gastroesophageal reflux disease (GERD), bilious vomitting (94%)(2-6) and etc. which can be associated with DGR.
This excessive pathologic presence of biliary intestinal content in the stomach and also esophagus lumen, may be the underlying causative “arche”; the “ultimate principle” of significant co-morbidities such as gastritis, gastric ulcerations, pernicious anemia, erosive esophagitis(9), Barrets metaplasia/dysplasia(7), gastric polyps(8), post cholecystectomy syndrome/reflux(11) and even gastric carcinoma(10, 12-19).
Alkaline Reflux and Predisposition to Cancer
Bile acid is considered as an important mucosal toxic factor triggering the injury of gastric mucosa(12). In an animal study conducted by Kuwahara et.al., the bile, the main component of the duodenal juice, has been implicated in gastric cancer due to duodenogastric reflux, at the remnant stomach of rats after gastrectomy(13). In humans, duodenogastric reflux also has a role in gastric stump carcinoma(14). Studies have shown that bile acid was associated with intestinal metaplasia in the cardia(15) and with the degree of esophageal mucosal injury(16). Several clinical studies have emphasized the role of chronic duodenogastroesophageal reflux in the development of Barrett esophagus with intestinal metaplasia(17,18). Komichi et. al. reported that the bile acid caused DNA damage, which may contribute to the carcinogenesis(19).
Life with Duodenogastric Reflux (DGR)
DGR is a complex unity of a vast number of pathologies and provoke a painful and disturbing daily life for most time. Patients mostly refer to gastroenterologists, surgeons, dietitians and even pschiatrists to find a solution in any way. Nevertheless, as in most cases, many studies confirm the inefficacy of medical treatment and life style modifications. Cholestyramine(20) and Sucralfate(21) are two main medical agents but both are unsuccessful in longterm relief of symptoms.
Many patients have to face unconcernedness at their families, their friends and even their doctors:
“I do not think you have bile reflux!”,
“Bile reflux does not cause these symptoms!”,
“Definitely you do not have bile reflux. Anybody can vomit bile sometimes. Do not urge yourself.”
and even
“Have you ever considered to see a psychiatrist for your discomfort?!”.
The main issue for many of the patients is the scientific or professional ignorance of their physicians. Many specialists such as surgeons, internalists even gastroenterologist do not intend to treat objective bile in the stomach that is present during endoscopy. If the patient has no sypmtoms than, may even do not report it. Or biliary intestinal content may not be seen objectively at the time of endoscopy. So further investigation at symptomatic patients should be done to diagnose the underlying pathology.
Diagnostic Evaluation for Duodenogastric Reflux
Endoscopy
The first step for any upper gastrointestinal complaint should be an endoscopic evaluation of esophagus, stomach and duodenum as possible. Video enhanced magnified observation of intraluminal space gives a direct and clear evidence of any on going pathology and also provides a wide opportuinity to diagnose and treat most of these problems.
If a biliarypancreatic reflux is present, it can be observed whether it is in phsysiologic limits or in a pathologic amount. For severe or massive biliary pooling in stomach, mainly there is no need for further evaluation. Medical treatment, dietary modifications, and standart reflux life style recommendations should be given to the patient. If the complaints do not reveal in 3-6 months interval; we recommend to perform another endoscopy. The presence of bile after medical treatment may be an indication for De Meester Switch Surgery to surgically divert the biliary intestinal juice away from stomach and preserve gastric mucosa from further schimic trauma.
Bilitec 2000 Ambulatory Bile Reflux Monitor(22)
Bilitec 2000 is an innovative device used to detect the amount of bilirubin in esophagus/stomach. It spectrophotometrically detects the bilirubin in the reflux material. It is able to monitor the esophagus and stomach for 24 hours by means of the exposure time of mucosa to bilirubin-containing bilio-intestinal reflux material.
The probe extends to 5 cm below the esophago-gastric junction; its different than Impedence pH Meter application. But, although giving brief information about the exposure time, it is not able to detect the pH.
The diet needs to be standardized in order to avoid false positive results due to the ingestion of foods with absorption close to bilirubin absorption.
When combined with pH Monitoring, 4 types of reflux can be evaluated:
- Simultaneous increase in absorbance and pH (mild alkaline reflux)
- Increase in bilirubin with unchanged pH (biliary reflux with non alkaline pH)
- pH increase with unchanged absorbance (mild alkaline but non biliary reflux)
- Both unchanged (acid reflux).
The Bilitec 2000 might have up to 23 % false negative result and may fail to detect the biliary reflux(23). False positivity is significantly low and can be controlled easily with Impedance-pH Meter. If the Bilitec does not show the reflux in a symptomatic patient, further investigation should proceed with 24-Hour Esophageal Impedance-pH Meter.
The biliary alkalene reflux and non-acidic reflux are two different phenomenons that need special differential diagnostic evaluation(24).
24-Hour Esophageal Impedance-pH Meter
Impedance measurement is mainly used to detect GERD (Gastro Esophageal Reflux Disease) and distinguish acid and weakly acidic refluxes at the esophagus causing symptoms.
Gastro-Esophageal Reflux Disease (GERD) is caused by the reflux of gastric contents into the esophagus. That’s why, impedence may not be effective to diagnose the alkaline reflux if it does not extend to esophagus.
Impedence simply detects the extend of the reflux in the esophagus lumen. It distinguishes whether distal or proximal in esophagus. When it is combined with a pH sensor at the very distal tip, the nature of the reflux material can be also detected. Also with 24 hour monitorisation, day and night difference can be observed.
Non of the tests above can specifically diagnose biliary reflux and can differentiate from other types of reflux and GERD. For every patient a through evaluation with detailed history of disease and complaints; previous treatments and tests. The further evaluation might need a combined use of previously mentioned diagnostic tools.
Basis of Treatment
Treatment of alkaline and acidic reflux are almost the same.
The basis of reflux treatment should be patient education such as;
- Stop smoking,
- Do not eat before sleep,
- Loose weight if you need
The so called Life Style Modification is a must at the beginning of Duodenogastric Reflux just as treatment of GERD.
Medical treatment is also shares the same armomentary with GERD:
- Drugs that decrease the acidity of stomach like Proton Pump Inhibitors; however use of ppi is controversial according to some physicians due to non-acidic nature of DGR. But still it has a wide range of use due to difficulty of differentiation of alkaline and acidic reflux symptoms.
- Prokinetic drugs such as metaclopromide, may influence the gastric emptying decreasing the biliary reflux.
- Sucralfate to cover the esophageal and stomach mucosa to prevent the mucosal injury of bile.
It’s well known that life style changes and medical treatments are not quite enough for relief of symtoms and also do not effectively prevent the bile coming to stomach.
Surgical Treatment –
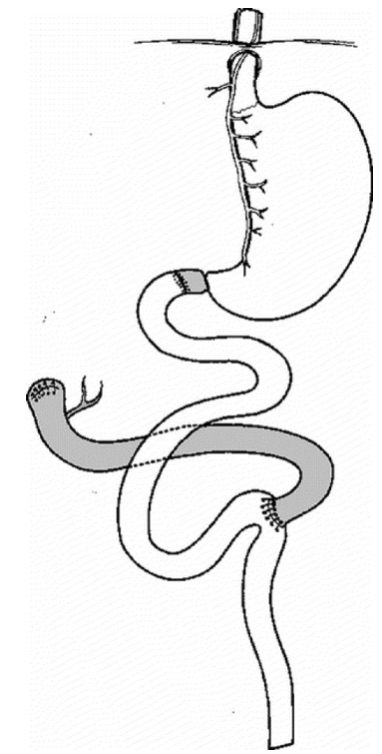
The De Meester Switch Surgery
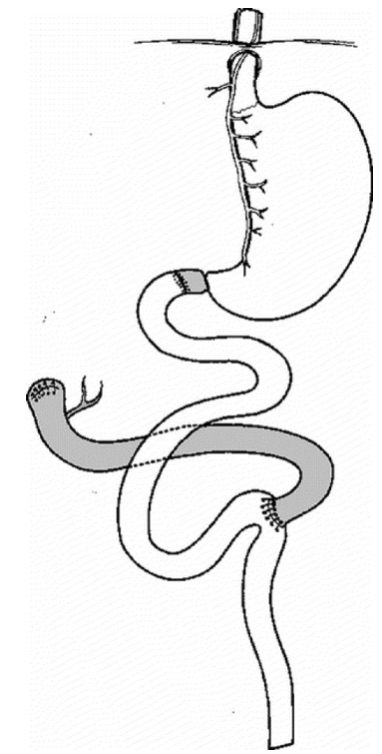 Dr. De Meester proposed a surgical techique in 1987 to anatomically divert the biliary pancreatic juice away from stomach without breaking the integrity of the gastropyloric physiology(25). The De Meester Switch procedure is the gold standart treatment of Duodenogastric Reflux with 100 % diversion of duodenal biliopancreatic juice away from stomach. Strignano P. and colleagues reported results of De Meester Switch in 48 patients with 81 months of median follow-up with almost excellent results over duodenogastric reflux and its symptoms(26).
Dr. De Meester proposed a surgical techique in 1987 to anatomically divert the biliary pancreatic juice away from stomach without breaking the integrity of the gastropyloric physiology(25). The De Meester Switch procedure is the gold standart treatment of Duodenogastric Reflux with 100 % diversion of duodenal biliopancreatic juice away from stomach. Strignano P. and colleagues reported results of De Meester Switch in 48 patients with 81 months of median follow-up with almost excellent results over duodenogastric reflux and its symptoms(26).
After a follow-up period ranging from 3 to 174 months (median, 81 months), 29 patients (60.4%) had no residual gastric symptoms, preoperative gastric symptoms were improved in 16 patients (33.3%), 2 patients (4.2%) were not improved at all, and 1 patient had experienced symptomatic recurrence after a 92-month symptom-free period (2.1%). Overall 93.7 % of patients had full or significant remission of disease.
Advantages of De Meester Switch over R-Y Gastric Bypass
R-Y Gastric Bypass (RYGB) mainly diverts bile and acid from esophagus but especially if the remnant stomach stays untouched, the biliary reflux continues to the remnant stomach. The GERD related symptoms might have a relief after RYGB but the mucosal damage of bile in the remnant stomach stays and continues as it is. RYGB is preferred by many surgeons for its easy applicability and short learning curve. However, it does not divert the bile effectively from stomach. Moreover if the remnant stomach is left, than the patient looses his/her chance to endoscopic evaluation of the stomach.
The De Meester Switch preserves the stomach integrity in continuation with pyloric valve. It diverts the duodenal biliopancreatic juice 100 to 150 cm away from stomach and definitely prevents the bile coming up to gastric lumen.
No Malabsorption!
The most important concern of our patients is whether they will have a malabsorption after De Meester Switch Surgery. It is due to the close proximity of Duodenal Switch to De Meester Switch Surgery. the Duodenal Switch is a highly effective and severely malabsorptive bariatric/metabolic surgery which is preferred in long term treatment of super obesity. Duodenal Switch bypasses almost 2/3rd of small intestines leaving 250-300 cm of intestines for absorption. This means average 500-600 cm of intestines are bypassed in Duodenal Switch forming a significant fat and calorie malabsorption.
De Meester Switch Surgery is completely different than Duodenal Switch by means of absorption and risk of malabsorption. De Meester Switch Surgery bypass only 40-50 cm of jejunum. That means Duodenal Switch is 10 folds malabsorptive however De Meester Switch Surgery has no significant malabsorption. Only iron deficiency might be a risk for some patients at the early periods of De Meester Switch Surgery. All of the patients can over come the iron deficiency with their fully preserved stomach capacity.
De Meester Switch Surgery is the most effective and durable treatment option of non-compliant persistent duodenogastric reflux. The surgery is performed totally laparoscopic. The quality of life increases at the day of operation and medications can be stopped in 3 months post operative.
References
- Byrne JP, Romagnoli R, Bechi P, et al. Duodenogastric reflux of bile: a range of normal values in healthy controls using the Bilitec 2000. Physiol Meas. 1999;20:149–158.
- Ritchie WP. Alkaline reflux gastritis: late results on a controlled trial of diagnosis and treatment. Ann Surg 1986; 203:537-544
- Gowen GF. Spontaneous enterogastric reflux gastritis and esophagitis. Ann Surg. 1985;201:170–175.
- Warshaw AL. Bile gastritis without previous gastric surgery: contribut- ing role of cholecystectomy. Am J Surg. 1979;137:527–531.
- Ritchie WP. Alkaline reflux gastritis: an objective assessment of its diagnosis and treatment. Ann Surg. 1980;192:288 –298.
- Hermans D, Buts JP, Collard JM, et al. Primary duodenogastric reflux in children and adolescents. Eur J Pediatr. 2003;162:598 – 602.
- Romagnoli R, Collard J-M, Serra A-M, etal. Is the DGR Bilitec® profile different in GERD patients with and without Barrett’s esophagus? In: Giuli R, Scarpignato C, Collard J-M, et al. Eds. The Duodenogastroesophageal reflux. Paris: John Libbey, 2006;445–449.
- Mabrut JY, Romagnoli R, Collard J-M, et al. Familial adenomatous polyposis predisposes to pathological exposure of the stomach to bili- rubin. Surgery. 2006;140:818–823.
- Romagnoli R, Collard JM, Bechi P, et al. Gastric symptoms and duodenogastric reflux in patients referred for gastroesophageal reflux symptoms and endoscopic esophagitis. Surgery. 1999;125:480 – 486.
- Domellöf L. Gastric carcinoma promoted by alkaline reflux gastritis -- with special reference to bile and other surfactants as promoters of postoperative gastric cancer. Med Hypotheses. 1979 Apr;5(4):463-76.
- Ahmet Uyanikoglu, Filiz Akyuz, Fatih Ermis, Serpil Arici, Gurhan Bas, Mustafa Cakirca, Bulent Baran and Zeynel Mungan. Does Cholecystectomy Increase the Esophageal Alkaline Reflux? Evaluation by Impedance-pH Technique. J Neurogastroenterol Motil, Vol. 18 No. 2 April, 2012 pISSN: 2093-0879 eISSN: 2093-0887. http://dx.doi.org/10.5056/jnm.2012.18.2.18
- Bernstein H, Bernstein C, Payne CM, Dvorakova K, Garewal H. Bile acids as carcinogens in human gastrointestinal cancers. Mutat Res 2005;589:47–65
- Kuwahara A, Saito T, Kobayashi M. Bile acids promote carcinogenesis in the remnant stomach of rats. J Cancer Res Clin Oncol 1989;115: 423–28.
- Kondo K. Duodenogastric reflux and gastric stump carcinoma. Gastr Cancer 2002;5:16–22.
- Dixon MF, Mapstone NP, Neville PM, Moayyedi P, Axon ATR. Bile reflux gastritis and intestinal metaplasia at the cardia. Gut 2002;51: 351–5.
- Nehra D, Howell P, Williams CP, Pye JK, Beynon J. Toxic bile acids in gastro-oesophageal reflux disease: influence of gastric acidity. Gut 1999;44:598–602.
- Gillen P, Keeling P, Byrne PJ, Healy M, O'Moore RR, Hennessy TP. Implication of duodenogastric reflux in the pathogenesis of Barrett's oesophagus. Br J Surg 1988;75:540–3.
- Iftikhar SY, Ledingham S, Steele RJ, Evans DF, Lendrum K, Atkinson M, et al. Bile reflux in columnar-lined Barrett's oesophagus. Ann R Coll Surg Engl 1993;75:411–6.
- Komichi D, Tazuma S, Nishioka T, Hyogo H, ChayamaK. Glycoche- nodeoxycholate plays a carcinogenic role in immortalized mouse cholangiocytes via oxidative DNA damage. Free Radic Biol Med 2005;39:1418–27.
- Meshkinpour H, Elashoff J, Steward H, et al. Effect of cholestyramine on the symptoms of reflux gastritis: a randomized, double-blind, cross-over study. Gastroenterology. 1977;73:441– 443.
- Buch KL, Weinstein WM, Hill TA, et al. Sucralfate therapy in patients with symptoms of alkaline reflux gastritis: a randomized, double-blind study. Am J Med. 1985;79:49 –54.
- Bechi P, Cianchi F. Technical aspects and clinical indications of 24-hour intragastric bile monitoring. Hepatogastroenterology. 1999 Jan-Feb;46(25):54-9.
- Barrett MW, Myers JC, Watson DI, Jamieson GG. Detection of bile reflux: in vivo validation of the Bilitec fibreoptic system. Dis Esophagus. 2000;13(1):44-50.
- Pace F, Sangaletti O, Pallotta S, Molteni P, Porro GB. Biliary reflux and non-acid reflux are two distinct phenomena: a comparison between 24-hour multichannel intraesophageal impedance and bilirubin monitoring. Scand J Gastroenterol. 2007 Sep;42(9):1031-9.
- Demeester TR, Fuchs KH, Ball CS, et al. Experimental and clinical results with proximal end-to-end duodenojejunostomy for pathologic duodenogastric reflux. Ann Surg. 1987;206:414 – 426.
- Strignano P., Collard JM. et al. Duodenal Switch Operation for Pathologic Transpyloric Duodenogastric Reflux. Ann Surg 2007;245: 247–253
 English
English Turkish
Turkish